Case
A 45-year-old man presented to the ED with severe left leg pain after he was struck by a sports utility vehicle while driving his moped. A radiograph of the affected extremity was taken in the trauma bay (Figure 1a). During the initial evaluation, it was noted that the patient had no pulses in his left foot.
What is the suspected diagnosis?
What would be the next imaging test (if any) that should be performed?
Answer
The radiograph of the knee demonstrates acute comminuted fracture (arrows, Figure 1b) of the distal metadiaphysis of the left femur with angulation and marked posterior displacement of several of the fracture fragments. In a patient with evidence of vascular compromise, an injury to the femoral or popliteal arteries should be considered.
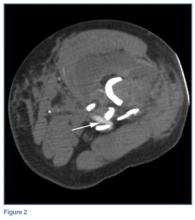
Since this patient required computed tomography (CT) of the abdomen and pelvis, a CT angiogram (CTA) of the left leg was also ordered. The axial CTA image demonstrated acute angulation/compression of the femoral artery (white arrow, Figure 2) at the level of the adductor canal due to adjacent angulated/displaced fracture fragments. Three-dimensional reconstructed image from the CTA further delineated this acute arterial angulation/compression of the femoral artery (white arrow, Figure 3) There was no evidence of contrast extravasation to indicate vessel rupture or pseudoaneurysm formation.
Fractures of the distal femur are relatively uncommon, accounting for 3% of femoral fractures and only 0.4% of all fractures.1 These fractures tend to occur predominantly in young men after a high-impact injury or in elderly women following a low-impact injury. Common mechanisms causing distal femur fractures in younger patients are motor vehicle collisions—especially involving motorcycles or mopeds—or falls from heights. In elderly patients, the mechanism is often a fall onto a flexed knee; in these cases, the fractures are often preceded by other age-related fractures or signs of osteopenia.2The femoral artery is well protected by musculature as it travels caudally down the leg. It enters the adductor canal at the femoral triangle just inferior to the inguinal ligament. It stays medial to the femoral shaft and exits the adductor canal at the adductor hiatus within the adductor magnus muscle. Upon exiting the adductor canal at the level of the femoral metadiaphysis, the artery travels into the popliteal fossa posterior to the knee, where it becomes the popliteal artery. It is within the popliteal fossa that the artery is most susceptible to injury. The risk of arterial injury increases significantly if the knee is dislocated posteriorly.3 The patient in this case likely avoided serious arterial injury due to the fact that his knee joint remained aligned.
Regarding treatment, the patient was taken to the operating room for external fixation to stabilize the fracture. The pulses returned with reduction of the fracture. The extent of arterial and soft-tissue injury was investigated and no significant arterial damage was noted.
In most fractures of the distal femur, a CT scan of the leg is recommended to exclude intra-articular involvement. If there is clinical suspicion of vascular injury, the diagnostic options include CTA, catheter angiography, or surgical exploration. In most centers, CTA is the fastest, the most cost-effective option, though imaging studies should not delay the surgical intervention of a frankly ischemic limb. Vascular imaging should always be performed in patients who suffer a dislocation of the knee joint, as these patients have a 30% to 40% risk of arterial injury.4
Dr Daniels is a postgraduate year 2 resident in diagnostic radiology at New York-Presbyterian Hospital/Weill Cornell Medical Center, New York City. Dr Bartolotta is an assistant professor of radiology at Weill Cornell Medical College in New York City and assistant attending radiologist at New York-Presbyterian Hospital/Weill Cornell Medical Center. Dr Sy is an assistant professor of clinical radiology at Weill Cornell Medical College, and an assistant attending radiologist at New York-Presbyterian Hospital-Weill Cornell Campus, New York City. Dr Hentel is an associate professor of clinical radiology at Weill Cornell Medical College in New York City. He is also chief of emergency/musculoskeletal imaging and executive vice-chairman for the department of radiology at New York-Presbyterian Hospital/Weill Cornell Medical Center; and associate editor, imaging, of the EMERGENCY MEDICINE editorial board.